Marketing Autorisation Extension versus type II variation.
Legal basis:
When marketing authorization holders wish to register a medicine in Europe, they submit a marketing authorisation (MA) application to the health authorities.
Once marketing authorisation has been obtained, it is the responsibility of the marketing authorisation holder to keep the dossier up to date and to report any changes that affect the marketing authorisation. These changes may be of various types (administrative, quality, safety). To do this, the marketing authorisation holder must submit a notification or a variation application to the competent health authorities.
A variation is a modification to the marketing authorisation.
There are also other types of MA modifications, known as MA extensions.
Changes to the terms of a European marketing authorisation are provided for in Directive 2001/83/EC and Regulation (EC) No 726/2004, and detailed in Regulation (EC) No 1234/2008 on the examination of variations to the terms of marketing authorisations for medicinal products for human use (hereinafter referred to as the ‘Variations’ Regulation). New guidelines to facilitate the interpretation and application of the Variations Regulation were published in the Official Journal on 22 September 2025 and are applicable on 15 January 2026. The Annex to these guidelines provides details of the classification of variations. These guidelines cover the following categories of variations, defined in Article 2 of the Variations Regulation:
— Minor variations of Type IA,
— Minor variations of Type IB,
— Major variations of Type II,
— Extensions,
— Urgent safety restrictions.
Any modification must be classified in one of the above categories. However, in some cases, the distinction between a Type II (major) variation or an extension is complex.
Definitions:
- Type II variations
Type II variations are considered as major variations. These are variations which are not extensions of marketing authorisations and may have a significant impact on the quality, safety or efficacy of the medicinal product concerned. This type of variation is generally assessed within 60 days, but shorter assessment periods (30 days for safety-related variations) or longer periods (90 days for indication extensions) may be necessary.
- Extensions
Certain changes to a marketing authorisation must be considered as fundamentally altering the terms of that authorisation and therefore cannot be granted through a variation procedure. Annex I of the Variations Regulation sets out a list of changes to be considered as extensions; the two main changes requiring an extension are:
– Changes to the active substance(s):
– Changes to strength, pharmaceutical form and route of administration
According to Article 19 of the « modification » Regulation, an application for an extension shall be evaluated and granted in accordance with the same procedure as for the initial marketing authorisation to which it relates.
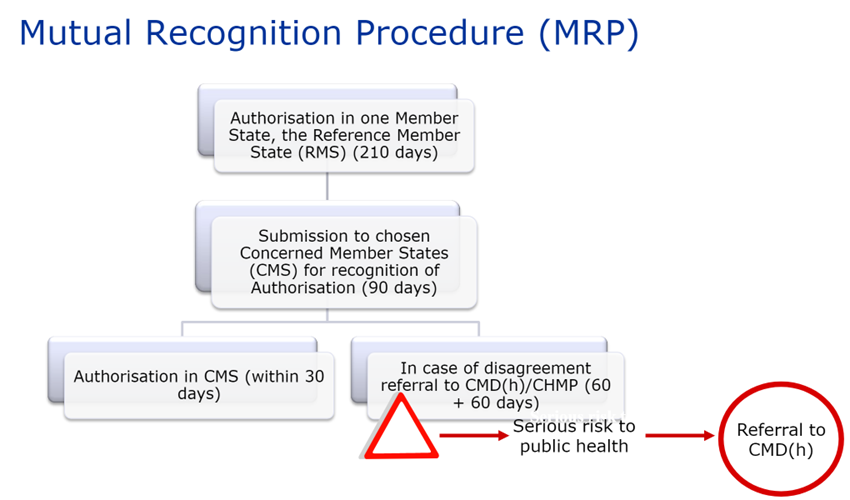
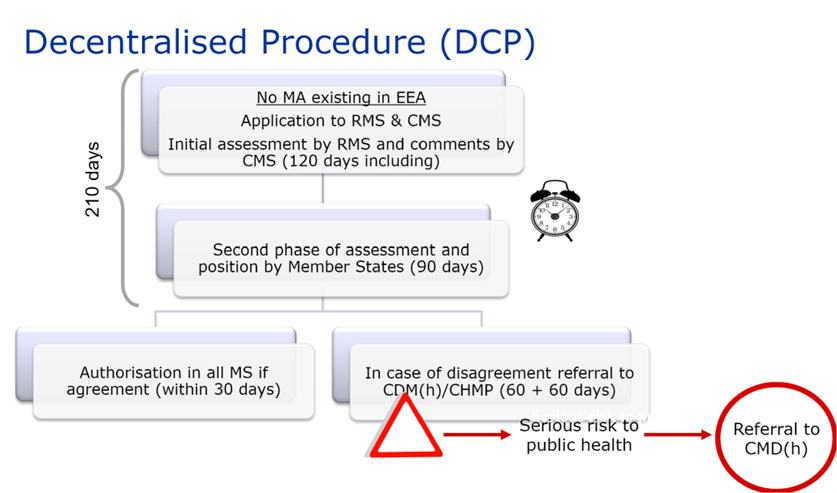
The extension may either be granted as a new marketing authorisation (national procedures, MRP and DCP) or included in the initial marketing authorisation to which it refers (centralised procedure).
In all cases, the new MA obtained is part of the global marketing authorisation and is not eligible to additional data protection (except in cases of ‘significant’ indication extensions based on comparative data).
The assessment timetable for an extension is the same as that for an initial marketing authorisation application.
In practice
Experience has shown problems in the classification of extension applications versus variations particularly regarding the items pharmaceutical form and strength. The « GUIDELINE ON THE CATEGORISATION OF EXTENSION APPLICATIONS (EA) versus VARIATIONS APPLICATIONS (V) » (Revision 4 – July 2019), proposes a harmonised and agreed interpretation of the Standard terms, with the aim of facilitating the application of the Regulation on variations throughout the EU and helping in the classification of requests.
The main principles of classification of extensions versus type II variations are as follows:
| Type of changes | |||||
| Pharmaceutical form | Strength | Presentation | Route of administration | Inclusion of medical devices | |
| Variation | Deletion of a pharmaceutical form | Deletion of a strength | Change or deletion of a pack size Change of fill volume | Addition or replacement of a measuring or administration device (part of the primary packaging)* | |
| Extension | Change of addition | Different strength or any other changes to the active substance(s) | Change or addition of a route of a route of administration | ||
* : unless the modification results in a change to the strength, pharmaceutical form or route of administration.
The guideline also provides examples presented as table for more complex cases.
It is important to note that variation requests may be grouped together with a marketing authorisation extension request. The assessment period applied to variations will be that of the marketing authorisation extension.
In summary
Apart from the question of the regulatory classification of the application (variation or extension), numerous practical questions may arise when compiling the application:
– Will my brand name be affected?
– How should I submit my extension request?
– What data should I generate?
– Can I group extension submissions with other types of variations?
– Do I need to meet pediatric requirements in my extension application?
– How should I integrate this extension into the eCTD?
ATESSIA can assist you in developing your regulatory strategy and drafting your variation or extension application dossiers, regardless of the registration procedure.
This article was written by Anne-Valérie Angérard, senior regulatory affairs consultant.