The need for a paediatric regulation for medicines
The need for a paediatric regulation in the EU is born almost 30 years ago with the report that:
- Medicines were used in children based on empirical knowledge and off-label, with not approved adaptations of doses,
- Pharmaceutical forms were not adapted to the paediatric population,
- Clinical trials were not conducted in children to preserve this population from exposure to medicines under development,
- Very few medicines were developed in this limited specific population partly.
In 2000, the International Conference on Harmonisation published a dedicated guideline (ICH E11 – « Clinical Investigation of Medicinal Products in the Pediatric Population ») with the objective to promote clinical research in the paediatric population.
In parallel, from 1997, the European Commission launched initiatives with different stakeholders that led to the publication of the so-called paediatric regulation (Regulation No. 1901/2006/EC) on 12 Dec 2006 that came into force in Jan 2007.
European Requirements for the paediatric development of medicines
That regulation, which has been amended twice, created the paediatric committee (PDCO) within EMA but also set up a comprehensive regulatory framework with obligations and incentives for Applicants and Marketing authorisation holders.
From 2007, any new Marketing authorisation application must be accompanied with the proof of compliance to an approved Paediatric Investigation Plan (PIP) that describes the studies that will be conducted in the paediatric population and associated timelines.
This requirement is also applicable to medicinal products with a valid patent or protection for which new indication (paediatric or not) new pharmaceutical form or new route of administration will be submitted.
This requirement is applicable whatever the chosen procedure (National, Decentralised, Mutual Recognition and Centralised).
The PIP details the following:
- A calendar and specific measures to assess quality, efficacy and safety of the medicines in all subsets* of the paediatric population;
- Any measure that will be put in place to adapt the formulation to the paediatric population to enable a safer, more adapted easier use of the medicines in the paediatric population.
Template of the EU PIP is available on EMA Website and should be used by Applicant to support effective assessment of the PIP.
*ICHE11 defines the paediatric subsets as:
- preterm newborn infants
- term newborn infants (0 to 27 days)
- infants and toddlers (28 days to 23 months)
- children (2 to 11 years)
- adolescents (12 to 16-18 years (dependent on region))
In parallel, the paediatric regulation set up rewards and incentives for some situations to support the development of medicines in children :
- Scientific advice and protocol assistance linked to paediatric development are free of charge at EMA level;
- Extension* of the protection (Patent or Supplementary Protection Certificate) by 6 months for a product authorised across the EU and for which results of the paediatric studies planed in the PIP have been included in the MA dossier (and included in the product information).
- 2 additional years of market protection in case the results of the studies planed in the PIP are submitted in an application for an orphan medicinal products;
- Finally, it created the notion of PUMA: Paediatric Use Medicines Authorisation which has a 10-year market exclusivity period.
*in this case, the MAH must market the product in the paediatric indication within 2 years upon approval. These deadlines are made available with a list published on EMA Website.
This incentives and rewards can be completed by other national incentives that are not detailed here.
Finally, this regulation provides that Marketing-authorisation holders must submit the results of studies on authorised medicines conducted in children to the European Medicines Agency (EMA) or to national competent authorities in the European Union (EU) included or not in a PIP. From 2007, MAH are requested to submit clinical study results in the paediatric population within 6 month from the termination of the study. Modification of SmPC can be requested by the HAs based on those data.
Specific cases
There are cases where the inclusion of a PIP is not a prerequisite for the submission of a MA or above-mentioned post MA submissions or where some adaptations are possible.
Exemptions :
First of all, some MA are exempted from the requirement to perform a PIP. These legal basis are:
- Applications according to article 10*: Generic, Hybrid and Biosimilar
- Application according to Article 10a*: Well-Established Use
- Applications according to Articles 13 and 16*: Homeopathic and traditional herbal medicinal products
*of Directive 2001/83/EC
Waivers :
In addition, the regulators have considered cases where a PIP is not needed or requested:
- Medicines not expected to be efficient or safe in the paediatric population of subset of paediatric population,
- targeted disease does not exist in the paediatric population,
- no additional benefit expected in the paediatric population versus the already available treatment.
In those cases, class waivers or specific waivers are possible. For the first case, the PDCO publishes a list of class waivers that are applicable. For the second option, it is requested to submit a specific waiver request to the PDCO.
Deferrals :
Finally, the regulators also provided cases where the paediatric requirements is not requested to be performed before submission of the Marketing Authorisation Application: the PDCO may grant deferral.
Such situations are expected for scientific or technical reasons or on Public Health grounds or when clinical results in adults are necessary prior to administer the product to the paediatric population.
In the case of deferral, a detailed calendar agreed with the PDCO is approved and must be followed by the MAH. In addition annual reports on paediatric deferred measures must be submitted by the owner of the PIP.
These waivers and deferrals might concern the full paediatric population or only some subsets of the paediatric population.
Regulatory activities
Pre-MA
It is expected that PIP (initial version), deferral, product specific waiver requests, confirmation of applicability of class waiver are submitted to the PDCO via the IRIS portal. Paediatric regulation requests that these requests must be submitted at the latest at the date by when Pharmacokinetics studies are achieved.
PDCO will appoint a Rapporteur that will be in charge of the PIP assessment, product specific waiver or deferrals assessment within 60 days form validation. This period can be extended by a further 60-day assessment period as necessary. There is no fixed timelines for responses.
When a PIP is approved, the PIP becomes binding for the applicant that must submit PIP modifications if relevant (e.g. delayed timelines).
MA and Post MA Regulatory activities
Before submission of a MA for which a PIP is mandatory or for which deferral has been approved, the applicant should submit a request for compliance check to the PDCO. The PDCO will assess this request within 60 days and provide the applicant with a statement to be included in the MA dossier. In not performed before, the PDCO can be included during the validation period of the MAA that could lead to delayed start of the procedure.
Results of paediatric studies, waivers and deferrals are included in the Product Information.
Regulatory perspectives
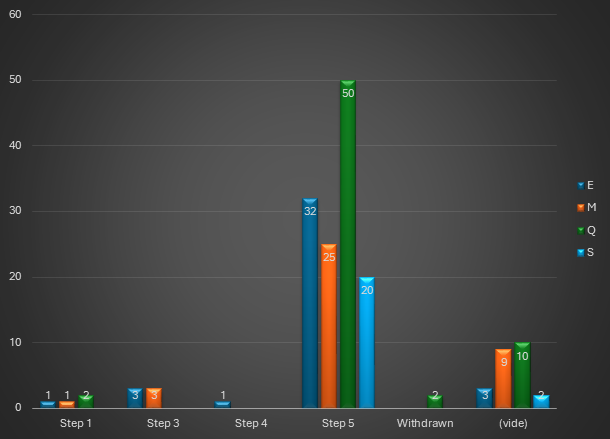
Some studies[i],[ii],[iii] (cf. references below) confirmed the positive impact of the paediatric Regulation on the availability of medicines for children. Nonetheless, needs to have medicines in children still exist.
It is also interesting to note that EMA developed an inventory of the needs for paediatric medicines that is available in their website to help developers to identify opportunities.
The revision of the pharmaceutical legislation in the EU includes a new regulation that will replace existing regulations including Regulation 1901/2006/EC. Among other changes, one of the intention from the Regulators is to bring a more strict framework of exemptions and thus increase the development of medicines in the paediatric population.
Atessia supports companies in defining paediatric strategy and writing PIPs.
This article was written by Agathe DAUBISSE, Senior Regulatory Affairs Advisor
[i] Toma M, Felisi M, Bonifazi D, Bonifazi F, Giannuzzi V, Reggiardo G, de Wildt S, Ceci A and TEDDY European Network of Excellence for Paediatric Research (2021) Paediatric Medicines in Europe: The Paediatric Regulation—Is It Time for Reform? Front. Med. 8:593281. doi: 10.3389/fmed.2021.593281
[ii] Nordenmalm S, Tomasi P, Pallidis C More medicines for children: impact of the EU paediatric regulation Archives of Disease in Childhood 2018;103:557-564.
[iii] : Volodina A, Shah-Rohlfs R, Jahn A. Does EU and US paediatric legislation improve the authorization availability of medicines for children in other countries? Br J Clin Pharmacol. 2023;89(3):1056‐1066. doi:10. 1111/bcp.15553