Centralised Procedure
The centralised procedure is defined by Regulation (EC) No 726/2004 of the European Parliament and of the Council of 31 March 2004 laying down Community procedures for the authorisation and supervision of medicinal products for human and veterinary use and establishing the European Medicines Agency (EMA).
This procedure allows obtaining a single marketing authorisation (MA), issued by the European Commission, valid in all Member States of the European Union as well as in the Member States of the European Economic Area (EEA): Iceland, Liechtenstein and Norway.
1/ Scope of application
The centralized procedure is mandatory for certain categories of medicines :
- advanced therapy medicinal products
- biotechnology medicinal products
- medicinal products containing a new, unauthorized active substance used in the treatment of acquired immunodeficiency syndrome (AIDS), cancer, neurodegenerative diseases, diabetes autoimmune diseases and other immune dysfunctions, and viral diseases
- orphan drugs.
It is optional for other categories of medicines which, although not mandatory, may be of interest at the European level. These include:
- medicines containing a new active substance that, as of 20 May 2004, was not authorized in the European Union
- medicines representing a significant therapeutic, scientific, or technical innovation
- medicinal products presenting an interest for patients at European Union level.
Generic medicines of a reference medicine authorised in the European Union may also be eligible for the centralised procedure.
2/ The actors involved
The Committee for Medicinal Products for Human Use (CHMP), the EMA’s scientific body, is at the core of the centralized procedure. To carry out its pharmacovigilance tasks, the CHMP relies on the scientific assessment and recommendations of the Pharmacovigilance Risk Assessment Committee (PRAC).
The main actors are :
- The applicant : the holder of the marketing authorisation application.
- The rapporteurs and co-rapporteurs : two Member States appointed by the CHMP to assess the application and draft the assessment reports.
- The CHMP : responsible for the scientific review and for providing an opinion on the benefit/risk balance of the medicinal product.
- The European Commission : the competent authority for the final marketing authorisation decision, based on the CHMP’s opinion.
3/ Timetable
The total duration of the scientific evaluation is 210 days, excluding clock stops to allow the applicant to answer questions from the CHMP.
Pre-submission
The applicant may arrange a pre-submission meeting with the EMA. These meetings are an essential opportunity to obtain procedural and regulatory advice from the Agency and to ensure that the application complies with the requirements of the centralised procedure.
Submission and validation
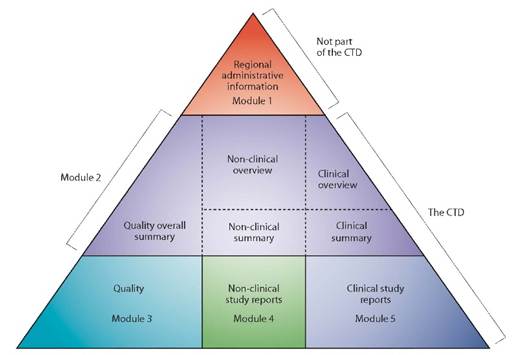
The complete dossier is submitted via the EMA portal. A technical validation is carried out, covering the dossier structure (eCTD), as well as a validation of the administrative and regulatory content. Once these validations are completed, the scientific evaluation officially begins on Day 1.
First evaluation (Day 1 to Day 120)
The rapporteurs and co-rapporteurs appointed by the CHMP carry out their initial scientific evaluation and draft a preliminary assessment report, consolidated with comments of the other members of the CHMP.
A peer review is then conducted by the rapporteur and co-rapporteur to harmonize opinions and finalize the list of questions to be addressed to the applicant. Day 120 marks the start of the clock-stop period, during which the applicant typically has up to three months to prepare its response document. Response time is not included in the 210 regulatory days.
Second evaluation (Day 121 to Day 210)
After the clock-stop period, the CHMP resumes the scientific evaluation based on the responses provided by the applicant (Day 121). This phase aims to verify that all questions have been adequately addressed and to finalize the Final Assessment Report (joint assessment) (Day 150).
If some questions remain unresolved or if a point requires clarification, the CHMP may hold a second clock-stop, during which the applicant provides additional information (Day 180).
After this second clock-stop, an oral explanation may be requested by either the applicant or the CHMP (Day 181). This hearing is generally held when the CHMP maintains major objections and allows the applicant to respond directly to the critical points raised by the committee.
Once all the answers to the questions have been received, the Final Assessment Report can be finalized and the CHMP adopts its final opinion on the benefit-risk balance of the medicinal product (Day 210). This opinion may be positive, adopted either by consensus or by an absolute majority of members, or negative. In the event of a negative opinion, the applicant has the right to appeal the decision in accordance with EMA’s procedures.
European Commission Decision
When the CHMP opinion is positive, the European Commission has 67 days to make the final decision on granting the marketing authorisation.
4/ In summary
The centralized procedure is the preferred authorisation route for innovative medicines seeking a European presence. It ensures a harmonized scientific evaluationassessment. However, its complexity requires solid strategic preparation and proven regulatory expertise.
| ATESSIA supports pharmaceutical companies in defining their registration strategy, preparing and submitting applications under the centralised procedure, and managing interactions with both the EMA and the European Commission. |
Article written by Lamya SAOUSSEN, Junior Regulatory Affairs and External Communication Advisor